Long COVID has, understandably, dominated our conversations about life after a virus. But here’s the thing—it’s not a new phenomenon. Not by a long shot. For decades, people have been grappling with mysterious, debilitating conditions that set in after a seemingly routine infection.
Their stories were often dismissed, their symptoms relegated to the shadows of “it’s all in your head.” The sheer scale of long COVID has finally forced the medical world to listen. It’s pulled back the curtain on a whole category of illness we’ve been largely ignoring: post-viral syndromes.
When Your Body Doesn’t Reset: What is a Post-Viral Syndrome?
Think of your immune system like a highly trained army. It fights off an invader—in this case, a virus—and then, ideally, stands down. With a post-viral syndrome, the army doesn’t get the memo. The battle is over, but the troops remain on high alert, causing collateral damage to your own body.
These conditions are chronic, complex, and often involve a multi-system breakdown. The initial infection is gone, but the body is stuck in a persistent state of dysregulation. The key symptoms often read like a frustratingly vague list:
- Crushing fatigue that isn’t relieved by sleep
- Widespread pain and muscle aches
- “Brain fog”—trouble with memory, focus, and finding words
- Unrefreshing sleep and disturbances
- Worsening of symptoms after minimal physical or mental exertion (a phenomenon called post-exertional malaise)
The Usual Suspects: Other Viruses That Can Trigger Chronic Illness
Long COVID’s most significant contribution might be validating the experiences of millions who got sick from other common viruses and never fully recovered. Let’s meet some of the other culprits.
Epstein-Barr Virus (EBV) and the Mononucleosis Link
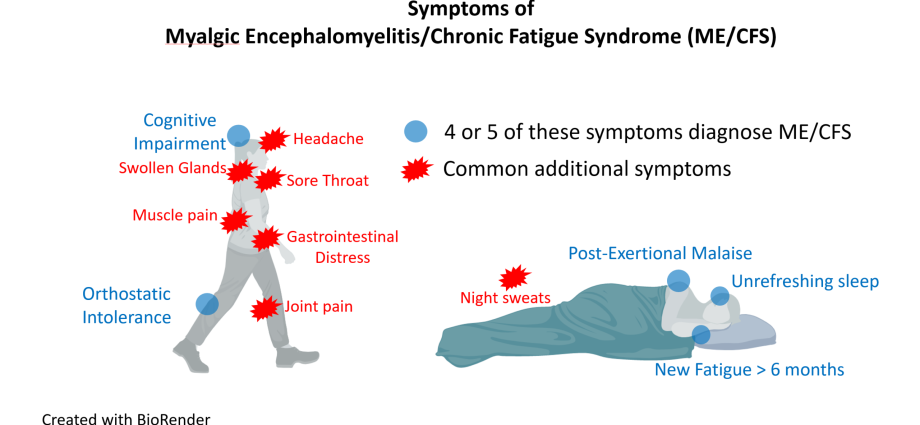
Almost everyone gets EBV. For most, it’s a mild childhood cold or a bout of teenage mononucleosis (“mono”) that they eventually bounce back from. But for a significant minority, the virus becomes a lifelong tenant. It can reactivate, and many researchers believe it’s a key trigger for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS).
The fatigue is… different. It’s not just being tired. It’s a profound, bone-deep exhaustion that rest doesn’t fix. And the post-exertional crash? It can feel like hitting a wall—a concrete wall—after even minor activity.
Enteroviruses and the Gut-Brain Connection
This family of viruses, which includes things like Coxsackievirus, often causes mild stomach bugs or summer colds. But they’ve also been implicated in the onset of ME/CFS. The theory is that these viruses can persist in the gut or central nervous system, quietly driving inflammation and disrupting everything from energy production to immune function.
Influenza: The Forgotten Aftermath
After the 1918 Spanish Flu pandemic, there were numerous reports of a “post-influenzal syndrome” that left survivors with chronic weakness and neurological issues for years. Sound familiar? Even today, a nasty bout of the seasonal flu can be the starting pistol for a long-term health decline for some individuals.
Connecting the Dots: Common Threads in Post-Viral Conditions
When you lay the symptoms of long COVID, ME/CFS, and other post-viral issues side-by-side, the overlap is staggering. It’s not a coincidence. Researchers are zeroing in on several shared mechanisms:
| Potential Mechanism | What It Means |
| Viral Persistence | Fragments of the virus hide in the body, keeping the immune system in a constant state of low-grade alarm. |
| Autoimmunity | The immune system gets confused and starts attacking the body’s own tissues. |
| Mitochondrial Dysfunction | The cellular power plants (mitochondria) are damaged, leading to a profound energy crisis. |
| Blood Clotting & Vascular Issues | Micro-clots and inflamed blood vessels impair oxygen delivery to tissues and organs. |
Honestly, it’s likely a messy combination of all these factors, unique to each person. The virus is the match, but the resulting fire depends on the individual’s genetic and biological tinder.
Navigating Diagnosis and the Road to Management
This is often the hardest part. There’s no single blood test for “post-viral syndrome.” Diagnosis is primarily clinical, based on a detailed history and the exclusion of other conditions. It can be a lonely and frustrating journey.
If you suspect you’re dealing with something like this, here’s a practical approach:
- Find a Believer: The first step is finding a healthcare provider who takes your symptoms seriously. Look for doctors familiar with ME/CFS, dysautonomia, or long COVID clinics—they’re often more equipped to connect the dots.
- Become a Detective: Keep a detailed symptom journal. Track your energy levels, sleep, food, and activities. This data is gold for identifying patterns and triggers, especially post-exertional malaise.
- Pace, Don’t Race: This is the cornerstone of management. It’s called “pacing.” You learn to live within your limited energy envelope, stopping before you hit your limit to prevent a crash. It’s counterintuitive in our “push through it” culture, but it’s essential.
- Address Specific Symptoms: Work with your doctor to manage the worst offenders—whether it’s sleep medication for unrefreshing sleep, medication for orthostatic intolerance, or cognitive strategies for brain fog.
A New Dawn for Post-Viral Illness
The silver lining of the long COVID tragedy is the unprecedented research momentum. We are learning more about the long-term effects of viral infections in five years than we did in the previous fifty. This isn’t just about SARS-CoV-2; it’s about rewriting the textbook on how we view infection and chronic disease.
The person who never recovered from mono in 2005, the one flattened by a stomach bug in 2010—their conditions are finally being seen as part of the same spectrum. It validates their suffering. It gives them a language to describe the indescribable.
We’re realizing that the goal isn’t always a triumphant “cure.” Sometimes, it’s about understanding the new rules of the body you now inhabit. It’s about management, about finding slivers of life and joy within new constraints. It’s about being believed. And for the first time, on a massive scale, that is finally starting to happen.