For decades, medicine has often operated on a one-size-fits-all model. You have high blood pressure? Here’s the standard pill. Feeling depressed? This is the usual first-choice medication. It’s a bit like walking into a shoe store and everyone, regardless of foot size, being handed the same pair of size eights. Sure, it might work for some, but for many, it’s going to be a painful, ill-fitting experience.
Well, that model is crumbling. We’re entering a new era, a revolution really, powered by our understanding of the human genome. This is the world of personalized medicine and its powerful engine: pharmacogenomics. It’s all about getting the right drug, at the right dose, to the right person at the right time. Let’s dive in.
What in the World is Pharmacogenomics?
Let’s break down that intimidating word. “Pharmaco” refers to drugs. “Genomics” is the study of genes and their functions. Put them together, and you have a field that explores how your unique DNA sequence affects your body’s response to medications.
Think of your body not as a generic machine, but as a custom-built workshop. Your genes provide the instructions—the blueprints—for all the tools (enzymes and proteins) that process medications. Pharmacogenomics is the science of reading those blueprints to predict how your workshop will handle a specific drug.
The Four Metabolic Types: A Genetic Traffic System
A core concept here is how you metabolize drugs. Imagine a pill traveling through your system. Your body needs to break it down and clear it out. The enzymes that do this job are genetically programmed. And honestly, we can generally categorize people into four main types:
| Metabolizer Type | What It Means | Potential Outcome |
| Poor Metabolizer | Slow breakdown of the drug. | Drug builds up, risk of side effects. |
| Intermediate Metabolizer | Slower than average breakdown. | May need a lower dose. |
| Normal Metabolizer | Standard, expected breakdown. | Standard dosing is usually effective. |
| Ultrarapid Metabolizer | Very fast breakdown of the drug. | Drug cleared too quickly, may not work. |
Knowing your type is a game-changer. For a poor metabolizer, a standard dose could be an overdose. For an ultrarapid metabolizer, that same pill might be little more than a sugar pill. This is the power of pharmacogenomics in action—it moves us from guesswork to precision.
Personalized Medicine in the Real World: It’s Already Here
This isn’t just futuristic speculation. Clinicians are using this knowledge right now to make better decisions. Here are a few powerful examples:
- Cancer Treatment: This is where personalized medicine truly shines. Certain cancers, like some types of breast and lung cancer, are driven by specific genetic mutations. Therapies can now be targeted to attack only cells with that mutation, sparing healthy ones and leading to fewer side effects compared to traditional chemotherapy.
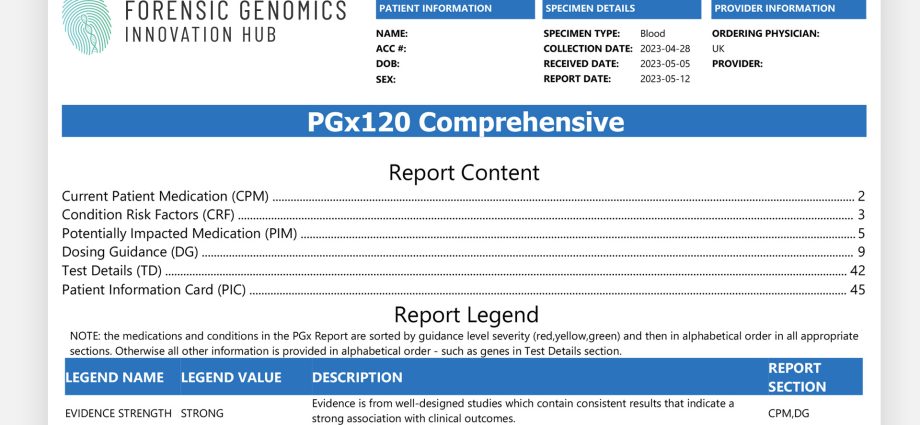
- Mental Health: Finding the right antidepressant or antipsychotic is notoriously difficult. It’s often a long, frustrating process of trial and error. Pharmacogenomic testing can provide clues about which medications a patient is likely to tolerate and which might be ineffective, potentially shaving months off the search for relief.
- Pain Management: Codeine, a common painkiller, is a prodrug. This means it needs to be activated by a specific liver enzyme (CYP2D6). Well, guess what? Ultrarapid metabolizers convert codeine to its active form, morphine, far too efficiently, which can lead to dangerous, even fatal, respiratory depression. Knowing this genetic info beforehand is critical.
- Cardiovascular Health: Clopidogrel (Plavix) is a blood thinner given to prevent strokes and heart attacks. But for poor metabolizers, the drug isn’t activated properly, leaving them at high risk for another cardiac event. A simple test can identify these patients so doctors can prescribe a different, more effective medication.
The Flip Side: Challenges on the Path to Personalization
It’s not all smooth sailing, of course. Widespread adoption faces some real-world hurdles.
Cost and insurance coverage is a big one. While the price of genetic testing has plummeted, getting it covered by insurance can still be a battle. There’s also the issue of interpreting the data. A genetic test result isn’t a simple “yes” or “no”; it requires expert analysis to be translated into a safe prescribing decision.
And then there’s the complexity of… well, human complexity. Your genes are a massive part of the story, but they’re not the whole story. Your age, diet, other medications, even your gut microbiome—they all interact in ways that can influence drug response. Pharmacogenomics gives us a huge piece of the puzzle, but not every single piece. Not yet, anyway.
What Does This Mean For You?
So, should you run out and get a pharmacogenomic test tomorrow? Maybe, maybe not. The most common and reliable use case is when a doctor is about to prescribe a medication with a known, significant pharmacogenomic link—like the ones we mentioned for blood thinners, painkillers, or certain mental health drugs.
If you’re starting a new long-term medication or have a history of bad side effects or medications just not working, it’s a conversation worth having with your doctor. You can ask, “Hey, is there a genetic test that might help us pick the best option here?”
The goal is to be proactive about your health. It’s about shifting from a passive recipient of care to an informed partner.
The Future is Written in Our Genes
We’re standing at the edge of a fundamental shift. The old model of “diagnose and prescribe” is being replaced by “predict and preempt.” Imagine a future where your electronic health record includes your pharmacogenomic profile. Before a doctor even writes a prescription, an alert could pop up: “Warning: Patient is a poor metabolizer for this drug. Consider alternative.”
This is the promise of personalized medicine and pharmacogenomics. It’s a move away from population-wide averages and toward the beautiful, intricate, and utterly unique individual that is you. It turns medicine from an art into a science, and frankly, a science that has your name written all over it.